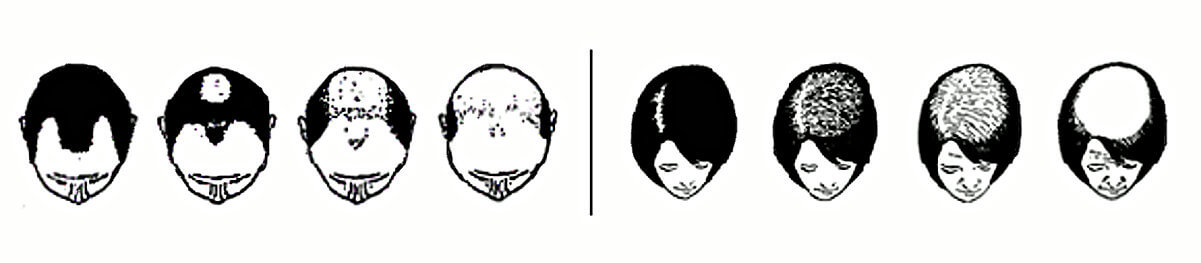
The term “cicatricial alopecia” or “scarring alopecia” refers to a diverse group of uncommon disorders that destroy hair follicles and associated sebaceous (oil) glands resulting in permanent hair loss. Although more commonly seen in women, scarring alopecia can occur in both sexes.
This destructive process may or may not be symptomatic; for example, in some cases, the hair loss is gradual with no symptoms, so the loss can go unnoticed for long periods; in other cases, the hair loss is rapidly progressive and associated with itching, burning and pain/discomfort.
Because the inflammation that destroys the follicle is below the skin surface, there is usually no visible “scar” on the scalp. Instead, one sees a smooth, shiny area devoid of hair follicles with the affected areas of the scalp showing little, if any, signs of inflammation. Less commonly, the inflammation can be marked with the patient experiencing redness, scaling, pustules, draining sinuses and increased or decreased pigmentation
Who is Affected?
Cicatricial alopecia occurs in both men and women. Although it can affect anyone of any age, it is not usually seen in children. A specific type of cicatricial alopecia called central centrifugal alopecia most commonly affects women of African ancestry and may occur in more than one family member. Most cicatricial alopecias are not contagious and, in general, they are not associated with other illnesses, but occur in otherwise healthy men and women. The majority of patients with cicatricial alopecia have no family history of a similar condition.
Diagnosis
While a hallmark of cicatricial alopecia is the absence of the openings of the hair follicles through which the hair fibers emerge from the skin, a scalp biopsy is essential to confirm the diagnosis. When performing a biopsy, it is important to select an area that still has some inflammation, as it is difficult to differentiate the various types of cicatricial alopecia in late-stage disease.
A hair-pull test is helpful in supporting the diagnosis and guiding the doctor where to biopsy. In a pull test, the clinician will grab onto a clump of hair in a region of active disease. The results of a pull test are based upon the number of hairs removed with each pull and by observing if the hairs contain intact follicles. A positive pull test will generally produce 5 or more hairs. It indicates active inflammation that is damaging and loosening the follicles from the surrounding tissue.
The type of inflammation seen on the scalp biopsy together with the overall pattern of the hair loss helps the doctor determine the specific type of cicatricial alopecia and its degree of activity. This allows the doctor to select the most appropriate therapy.
Other factors that help the doctor make a diagnosis and guide management include the following:
- The date of onset and rate of progression
- Specific symptoms – itching, pain, burning
- Any previous treatments
- Any hair regrowth – this would lead to an unlikely diagnosis of cicatricial alopecia
- Past medical history – any infections, diseases, or trauma
- Medications – including any exogenous androgens
- Hair treatments
- Family history – cicatricial alopecia rarely occurs in family members; other than central centrifugal alopecia
In addition, if pustules are present, the doctor may take cultures to identify which microbes, if any, may be contributing to the inflammation. However, as discussed, often there are few symptoms or signs and only the scalp biopsy demonstrates the active inflammation. Finally, the overall extent and pattern of hair loss should be photographed for future comparison.
Specific Conditions
Lichen Planopilaris (LPP)
Lichen planopilaris (LPP) is a type of scarring alopecia that presents in adulthood, mainly in females. Patients generally have a history of patchy hair loss with severe itching, pain, and burning. The course may be variable and may be seen as a slow progression of patchy hair loss or generalized hair thinning over several years, or a rapid progression over several months. LPP is generally considered a scalp hair manifestation of a disease process known as lichen planus. With lichen planus, there may be skin, nail, or mucous membrane involvement.
On examination of the patient with suspected LPP, the absence of follicular ostia (the openings of the hair follicles through which the hairs emerge from the skin) in the scalp is a strong indicator that this process is due to a scarring form of hair loss, and not to genetic hair loss. In LPP, there may be redness and irritation around the margins of the areas of hair loss, however, the center of the bare areas is smooth.
 Lichen planopilaris (LPP)
Lichen planopilaris (LPP)The scalp lesions may be single or multiple and can occur anywhere on the scalp. If LPP is suspected, a scalp biopsy will be performed to confirm the diagnosis.
The treatment is mainly directed toward patients with active disease progression. Therapy is aimed at preventing disease progression.
In general, medications such as hydroxychloroquine and mycophenolate mofetil are effective in reducing symptoms and signs of LPP. Even with resolution of the symptoms, there still may be progression of the hair loss in lichen planopilaris.
Frontal Fibrosing Alopecia (FFA)
Frontal fibrosing alopecia (FFA) is a scarring form of hair loss seen in predominantly women. A common complaint is recession of the hairline, often associated with loss of ones eyebrows. In contrast to common baldness (female pattern alopecia) where the hair actually thins, in FFA there are full thickness hairs interspersed with localized areas of balding. Once often sees a recession of the frontal hairline of about 1 inch associated with irritation and redness of the scalp, especially around the hair shafts. There usually is itching associated with this condition.
 Frontal Fibrosing Alopecia (FFA)
Frontal Fibrosing Alopecia (FFA)The skin along the receding hairline is generally pale and appears as a band that may progress above and behind the ears. The recession of the hair may be fast or slow – sometimes it is self-limiting.
The loss of eyebrows, which usually appears at the same time as the hairline recession (but may precede the hairline recession by years) can be complete or partial. Some patients may also complain of loss of eyelashes, or loss of hair on their arms or legs. These are all clinical signs supporting a diagnosis of FFA.
Following an initial history and physical exam, you doctor will generally perform a biopsy of your scalp. If a biopsy confirms the diagnosis of FFA, the next step is to discuss treatment strategies. The first line is medical management with oral medications such as hydroxychloroquinine and doxycycline, topicals such as corticosteroids, and intralesional injection of steroids. For loss of eyebrows, intralesional corticosteroids are used and repeated in 6 week to 3 month intervals. This may reverse the hair loss in patients who still have some remaining brows.
Central Centrifugal Cicatricial Alopecia (CCCA)
Central centrifugal cicatricial alopecia (CCCA) is a type of scarring alopecia that is typically seen in women of African descent, usually between the ages of 25 and 65 years. Although the cause is unknown, there may be a genetic predisposition in certain patients. This differentiates CCCA from the other scarring alopecias. It is unknown if aggressive hairstyling or grooming are the main causes of this condition, but heat, chemicals, and traction are suspected to play a role in CCCA.
Usually the symptoms are mild with occasional itching or tenderness but, at times, significant hair loss can occur before it is even noticed. Patients may first experience thinning over a small area of the central scalp which may gradually enlarge in a symmetric pattern to involve a larger area on the top and sides of the scalp. Very thin hairs may remain in the affected regions. On exam, the physician will generally check for hair breakage which is a sign of fragile hair that results from trauma to the hair shaft.
If there is no active inflammation on the biopsy, then medical management will likely not be effective. If a patient notes increased hair loss, with a biopsy showing inflammation, then oral medications as well as topical therapy may be useful. For patients who complain that their hair has stopped growing, it is useful to point out that the issue may be that the hair is breaking and it is fragile.
Hair care practices may need to be altered – such as eliminating hair braiding, chemical perms and excessive heat. This is an important point and may help to slow any progression of CCCA.
 Central centrifugal cicatricial alopecia (CCCA)
Central centrifugal cicatricial alopecia (CCCA)Treatment
- Oral medications
- 1st line: hydroxychloroquine, doxycycline
- 2nd line: mycophenolate mofetil, cyclosporine
- 3rd line: pioglitazone
- Topical medications
- Corticosteroids, topical tacrolimus, topical pimecrolimus, or Derma-Smoothe/FS scalp oil.
- Intra-lesional
- Triamcinolone acetonide (a corticosteroid) may be injected into inflamed, symptomatic areas of the scalp.
The patient continues treatment until the signs of scalp inflammation are decreased, and progression of the condition has been controlled. In other words, itching, burning, pain, and tenderness have cleared, scalp redness, scaling, and/or pustules are no longer present, and the hair loss has not extended. Surgical treatment for cosmetic benefit may be an option in some cases after the disease has been inactive for many years.
Prognosis
Cicatricial alopecias do not negatively affect ones general health. Although hair will not regrow once the follicle is destroyed, doctors can often treat the inflammation before too many follicles have been destroyed. For this reason, it is important to begin treatment as early as possible to control the inflammatory process. Often, there is sufficient hair in the surrounding areas to cover the affected scalp. Patients may also wear wigs, or hats, as this will not complicate the condition.
If you are concerned that you may have symptoms of a scarring alopecia or other forms of hair loss, it is important to see a qualified hair loss specialist as soon as possible.